Using AI to Treat Cancer: Improving Radiotherapy Planning
One half of the population of the United States and United Kingdom will be diagnosed with cancer at some point in their lives. Of those diagnosed, half will be treated with radiation therapy (or radiotherapy). Radiotherapy uses high-energy rays (like x-rays) to destroy or damage cancer cells and can be used by itself or in combination with other treatments (such as surgery, chemotherapy, and immunotherapy).
How Does Radiotherapy Work?
Radiotherapy treats cancer by using high-energy radiation to damage the DNA of cancer cells, inhibiting their ability to reproduce. This process involves either direct ionization of DNA atoms or indirect ionization through the creation of free radicals from water molecules, which then damage the DNA. Cancer cells, due to their rapid division and reduced DNA repair capabilities, are particularly susceptible to this damage. By precisely targeting tumors, radiotherapy aims to maximize damage to cancerous cells while minimizing exposure to surrounding healthy tissues.
Radiotherapy Planning
Radiotherapy (RT) planning is the process of creating 3D maps of tumors and the surrounding tissue which helps determine how high-energy x-ray machines (such linear accelerators) can deliver the radiation to kill the cancer. RT planning begins with acquiring high-resolution 3D CT or MRI scans of the patient’s body. Medical images such as MRI and CT are acquired as two-dimensional "slices" that are "stacked" on top of each other to create an "image volume." These stacks may contain hundreds of 2D slices which need to be analyzed.
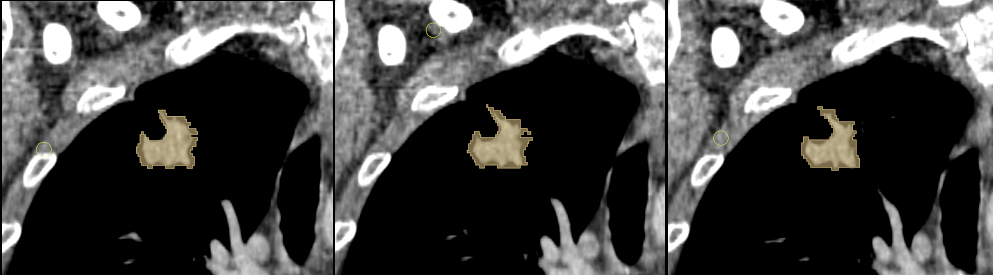
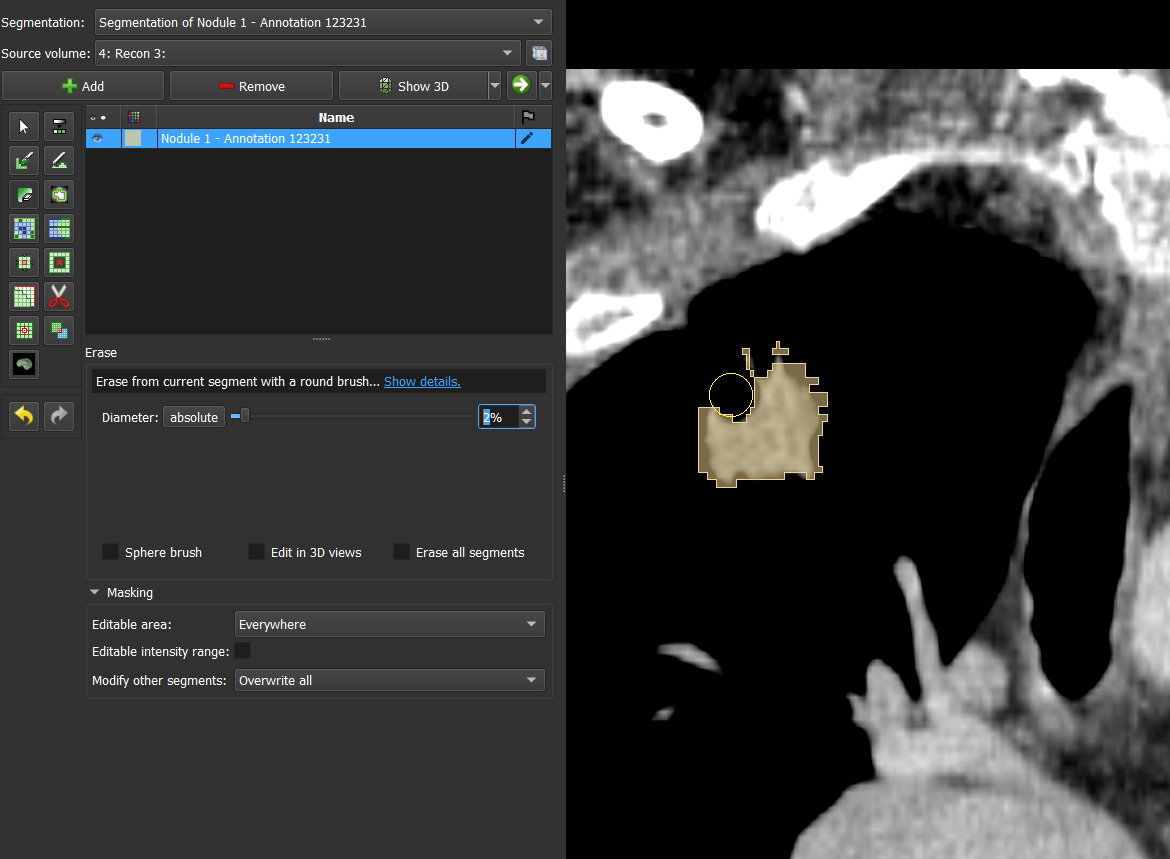
Each slice must be carefully reviewed by radiation oncologists or specialized technicians to identify anatomical structures, delineate any tumors that are present, and determine safe and effective radiation doses. Analyzing the images involves two critical steps:
- segmentation: isolating key anatomical structures and other regions of interest (ROIs)
- contouring: precisely outlining the tumor, which allows a map to be created for targeting radiation while avoiding healthy tissues
Segmentation provides a "pixel map" which assigns each pixel in an image to a structure of interest. Contouring is the process of converting the the pixel map to a 3D outline and tessellated model.
From Tedious to Timely
Artificial intelligence enables more efficient radiotherapy planning by improving the speed and consistency of segmentation.
Enhanced Efficiency
Manual segmentation and contouring requires that clinicians create an outline or use tools such as a "paintbrush" to label which pixels correspond to a tumor or organ on each slice. Once all the pixels are identified on one image, the same process is applied on the slices of the volume.
AI enabled segmentation solutions allow for clinicians to plan RT treatments in approximately one half to one third the time of manual segmentation software while also improving the consistency of the plans. The added efficiency reduces wait times for treatment and allows for more patients to access care. Timely treatment of cancer is particularly important since treatment delay provides the cancer time to grow and further metastasize.
More Consistent and Complete Segmentations
Two additional challenges in image segmentation are accurately and consistently labeling structures of interest and ensuring that all visible anatomy within a scan has been segmented.
The first of these issues is a consequence of the subjectivity of segmentation. There are often differences between segmentations created by different clinicians. This variability is one of the largest sources of uncertainty in treatment planning and can result in additional (potentially unneeded) treatment impacting patient health and incurring cost.
The second arises because segmentation is so time consuming. Each additional segmented structure adds significant work overhead to the radiologist or technician processing the scan. As a result, it is common that only the structures needed for treatment are identified and contoured with adjacent tissues unprocessed. Yet, applying contours to "organs at risk" (or OARs) provides a degree of protection by identifying the tissue so it can be included in the plan. Not creating contours leaves them at risk to damage from radiation.
AI based segmentation models, such as the Project Inner Eye (Microsoft) and Total Segmentator (University Hospital Basel) help mitigate both of these issues. Such models are trained on a broad set of data from many institutions, which helps to improve their consistency and generalization. They further support a large number of labels which allows for more complete labeling of healthy structures helping to ensure more complete contouring of at-risk tissue.
Models such as Total Segmentator allow for the segmentation of over a hundred structures on CT and MRI scans. Such broad support for many labels allow for highly detailed models, such as the torso above, to be created from a single scan.
Transforming Radiotherapy with AI
Radiotherapy planning is a cornerstone of effective cancer treatment, yet its reliance on manual segmentation and contouring has long posed challenges of time, consistency, and precision. With the advent of AI-driven technologies like Inner Eye and Total Segmentator, these obstacles are now being overcome. By streamlining workflows, reducing variability, and enabling more accurate treatment plans, AI not only empowers clinicians to deliver better care but also enhances patient outcomes by ensuring safer, more timely, and more effective radiation delivery.
As the integration of AI into radiotherapy planning continues to advance, the potential for personalized, and adaptive treatment grows. These tools represent an important step toward making cutting-edge cancer care more accessible for patients worldwide. Open source platforms such as Sonador (which is compatible with both Inner Eye and Total Segmentator) provide a pathway to help facilitate the adoption of these technologies, providing a pathway for healthcare institutions to address today's challenges as well as blaze a pathway to a future where cancer care is faster, smarter, and more reliable.
Comments
Loading
No results found